
*Advertisement – brand name mentioned
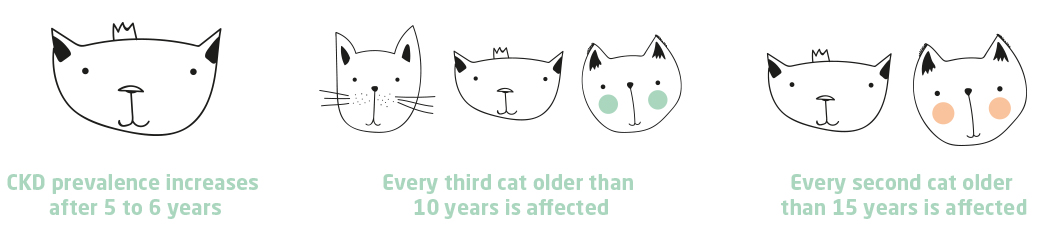
The field of human medicine shows extensive studies on the topic of chronic kidney disease in humans. It is assumed that about 10% of humanity is affected by CKD (chronic kidney disease). The comparable figure for cats with CKD is between 2 – 4% in relation to all cats (cat population). In older cats the numbers are much higher: one in three cats over 15 years of age can be expected to have CKD. The number of CKD afflicted individuals is thus on average higher in humans than in cats. This is mainly associated with unhealthy eating behaviours (e.g. diabetes).
Summary
- In human medicine, uraemic toxinsToxic, nitrogen-containing urinary substances responsible for uraemia and kidney damage.... are attributed as the cause of the high mortality of patients with chronic kidney disease
- Dialysis (blood washing) is not suitable for all waste products
- The reduction of renal toxins is therefore a broad research topic in human medicine
Underlying mechanisms of CKD
However, once the kidneys are diseased, the underlying mechanisms are very similar: In both cases, the number of functioning filter units (= nephronsNephrone sind die Filtereinheiten der Nieren....) decreases, as these perish irretrievably. These nephrons are, so to speak, the power plants of the kidneys. In these units, waste products are filtered out of the blood, toxins are actively excreted, hormones for blood formation and calcium and phosphate balance are formed, the water and electrolyte balance of the body is kept within very narrow limits and blood pressure is regulated.
The essence of CKD is precisely that the number of functioning nephrons decreases to such an extent that the kidneys can no longer fulfil all their aforementioned tasks. In addition, the loss of nephrons and thus of kidney function triggers various vicious circles that lead to further nephron destruction. CKD cannot be cured because these vicious circles cannot be stopped. Lost nephrons cannot heal and new ones are not formed. The number of nephrons thus decreases progressively. With the loss of nephrons, kidney output in turn continuously decreases, which further fuels the vicious circles. The treatment of CKD is about slowing down the progressive process of nephron destruction and thereby improving life expectancy and also quality of life.
System backlog
In affected humans and animals, the problem is that the diseased kidneys are no longer able to excrete all the waste products that arise. There is a backlog of urinary substances in the blood. In this case, blood washing (dialysis) helps to cleanse the blood of such substances. However, this is not successful with all urinary substances. Especially uraemic toxins, which are toxic waste products of protein metabolism, cannot be “washed out” due to their charge and remain in the blood. This is a comparable problem in human and veterinary medicine, where dialysis is rarely used.
Uraemic toxins in the crosshairs of mortality
In human medicine, these uraemic toxins, especially indoxyl sulphate, are considered to be the cause of the high mortality of patients with chronic kidney disease. Therefore, uraemic toxins are also called renal toxins. In feline medicine, too, this uraemic toxin is increasingly coming into focus in the context of CKD. The reason for this is that indoxyl sulphate is involved in a variety of processes that not only affect the kidneys themselves, but also other organs. Among other things, indoxyl sulphate, when it accumulates in the blood, leads to small foci of inflammation in the functional units of the kidneys. This leads to a connective tissue remodelling of these filter units with the consequence that they cannot maintain their tasks (see above) and perish. This further supports the progression of chronic kidney disease.

Indoxyl sulphate on the move
If the filtration capacity of the kidneys decreases, more indoxyl sulphate remains in the blood, so that the blood level of indoxyl sulphate increases. At the same time, more indoxyl sulphate reaches the organ tissues, where it can exert its toxic effect. Thus, more and more nephrons are lost and the vicious circle of progressive kidney destruction is further supported. This explains why indoxyl sulphate belongs to the so-called gut-kidney axis. The gut-kidney axis describes the connection between naturally occurring metabolic products in the gut (through the breakdown of proteins by the natural gut bacteria) and their harmful effects on the kidneys. In addition, there is the gut-brain axis and the gut-heart axis, each of which illustrates the negative effects of indoxyl sulphate on brain performance and heart function.
Rampant renal toxin
Indoxyl sulphate is formed from the natural protein metabolism. From the amino acid tryptophan, which is essential for cats (contained in many types of meat), the intestinal bacteria of the natural intestinal flora in the large intestine form the precursor indole. Indole passes from the intestine to the liver via the bloodstream. In the liver, indole is then converted into the actual uraemic toxin indoxyl sulphate. Indoxyl sulphate in turn reaches the kidneys via the bloodstream, where it is excreted in the urine. The excretion in the kidneys does not occur via filtration, i.e. the passive filtering out of the blood, but actively in the upper area of the long tubular system (proximal tubule). Therefore, this active excretion process can only be carried out by healthy nephrons.
At the same time, indoxyl sulphate leads to an increase in bacteria in the intestine that form indole from tryptophan. This not only leads to an imbalance of the intestinal bacteria (so-called dysbiosisImbalance of organisms of the the microbiome (all microbes on or within an animal’s tissues), for instance the imbalance of the intestinal flora as part of the microbiome....), but also increases the indoxyl sulphate blood level. Indoxyl sulphate is also found in the brain, where it can lead to cognitive impairment in CKD (gut-brain axis). Anaemia, hypertensionHigh blood pressure., diabetes and immunodeficiency, as well as elevated phosphate blood levels (hyperphosphataemiaIncreased phosphate in the blood.)* can be causally linked to elevated indoxyl sulphate blood levels. Uremic toxins, and in particular indoxyl sulphate, are considered to be responsible for the clinical signs of chronic kidney disease in humans and have also been discussed in cats in recent publications. In humans and also in cats and dogs, studies have shown a correlation between IRIS stages and indoxyl sulphate blood levels: The higher the indoxyl sulphate blood level, the more severe the CKD stage.
Human medicine – one step ahead?
Not only the quality of life of chronic kidney patients suffers under the influence of indoxyl sulphate. In humans, mortality also increases with rising indoxyl sulphate blood levels. The reduction of the kidney toxin is therefore a broad research topic in human medicine. While in veterinary medicine protein reduction in the feed (kidney diets) has been used for decades to counteract the increase in uraemic toxins in cats and dogs suffering from CKD, research in human medicine is already further advanced. Here, approaches are being researched to already reduce the indole formed in the intestine. The formation of indoxyl sulphate is thus prevented. This results in a reduction of the indoxyl sulphate blood level. This has positive consequences for kidney patients: Studies have shown a reduction in clinical symptoms and thus an increase in their quality of life, as well as a prolongation of life.
Oral adsorbers – A well-rounded approach
So-called OSCA (oral spherical carbon adsorbers) are suitable for this purpose. These are orally administered carbon spheres that can bind indole as a high-performance adsorber.
Indole accumulates on the inner surface of the spheres. The spheres are hollow on the inside and have a wide tube system. The tubes end on the outside in so-called micropores, whose diameter is very small. Uraemic toxins are very small molecules. Larger substances (e.g. vitamins) or even cells cannot pass through these pores. The uraemic precursors are then physically bound to the surface of the tube system. This works because the precursors of the uraemic toxins are charged. OSCA are therefore highly specific to uraemic precursors and only remove these.
In a new study over 8 weeks of treatment with OSCA, patients with a high degree of CKD, i.e. a late stage, showed not only higher indoxyl sulphate levels overall, but also the greatest reduction in indoxyl sulphate blood levels.
Transfer from human medicine to veterinary medicine
There is also an orally administered, spherical carbon adsorber (= OSCA) for cats. The active ingredient is called Renaltec®. According to the manufacturer, this product has been produced specifically for veterinary medicine. In studies on senior cats with elevated indoxyl sulphate blood levels, a significant reduction of the blood level could also be achieved after 8 weeks with the veterinary OSCA. In this respect, the studies in veterinary medicine are similar to those in human medicine. However, the reduction of the veterinary product is twice as high as that of the human OSCA.
The higher the reduction of the indoxyl sulphate blood level, the better for the kidney patients.
Bibliography:
- Kim, Sh., Jhee, J.H., Choi, H.Y. et al. (2020): New oral spherical carbon adsorbent effectively reduces serum indoxyl sulfate levels in moderate to advanced chronic kidney disease patients: a multicenter, prospective, open-label study. BMC Nephrology, 21, Artikel-Nummer: 317.
- https://porus.one/
*Blood levels of parathyroid hormoneParathyroid hormone (PTH) is a hormone secreted by the parathyroid glands, which regulates calcium levels in the blood. PTH is secreted in response to low blood calcium levels (hypocalcaemia). An increase in calcium concentration above the normal value inhibits PTH production (negative feedback). PTH stimulates... increase as blood levels of indoxyl sulphate increase. Parathyroid hormone (PTH) is feared in CKD. It is the cause of hyperphosphataemia and sets in motion a vicious circle of further kidney destruction. You can read more about this in my blog post “The devil is in the P“.



