
Kidneys are true powerhouses: they are excretory and detoxification organs and also have other important tasks for the body. Kidneys can filter waste products of metabolism and harmful substances (e.g. uraemic toxinsToxic, nitrogen-containing urinary substances responsible for uraemia and kidney damage....) from the blood and thus excrete them through the urine. They regulate the water balance as well as the body’s level of electrolytesElectrolytes are substances that produce an electrically conducting solution when dissolved in water, releasing mineral ions such as sodium, potassium, chloride and calcium. These ions can either be the positively or negatively charged or, combined as a salt, neutral.... and the acid-base balance. What is too much is excreted. As well as urinary substances that have to leave the body through the urine. In addition, the kidneys are also involved in blood pressure regulation and bone metabolism (calcium-phosphate balance).
Nephrons are the motors of the kidney
These valuable tasks are performed by the functional units of the kidneys, the so-called nephronsNephrone sind die Filtereinheiten der Nieren..... The nephrons are located in the outer kidney area, the renal cortex. Nephrons consist of very different parts that differ significantly in their appearance and function.
Each nephron consists of a glomerulum, a tangle of vessels enclosed by a sheath (Bowman’s capsule). The tangle of vessels consists of an afferent vessel (vas afferens) and an efferent vessel (vas efferens). In other words: one vessel that brings blood into the glomerulum and one that drains the filtered and thus “purified” blood out of the glomerulum. This is because the first excretory processes already take place here. With the help of the blood pressure and special filtration pores between the vascular tangle and Bowman’s capsule, it is ensured that mainly those substances leave the blood that should also be excreted – such as uraemic substances (e.g. ureaUrea is the nitrogen-containing breakdown product of protein metabolism. The nitrogen from the proteins is converted to ammonia in the liver, which is combined with carbon dioxide to form urea. This is continuously excreted via the kidneys but also via sweat. Urea is one of..., uric acid, ammonia). Important blood components such as proteins and red blood cells cannot pass through the filtration pores and therefore remain in the blood.
However, the increase in blood pressure can also influence the size of the filtration pores: if the blood pressure increases, the filtration pores become larger. This results in the excretion of proteins, so that more proteins are lost in the urine (proteinuriaIncreased protein in urine, leading to loss of protein. Normally, only a very small amount of protein is excreted in the urine. In chronic kidney disease, the amount lost may increase. High blood pressure damages blood vessels in the nephrons making them more permeable and...). With this glomerular filtration, more blood components are excreted than would be good for the body. Therefore, urine must be subsequently reprocessed in the nephron. Post-processing includes the recovery of important blood components (reabsorption) and also the active excretion of further blood components that were not or not sufficiently glomerularly filtered.
The counterflow principle of the tube system
Sodium, potassium and magnesium, because they are small molecules, also leave the blood and are filtered out with the other substances that are filtered out, such as phosphate, chloride, sugar, hormones or uraemic toxins and a lot of water. This first filtrate from glomerular filtration, also called primary urineThe initial urine entering the nephron due to filtration of the blood at renal corpuscles. It is not yet concentrated and does not contain any proteins...., enters the second part of the nephron. This second part of the nephron forms the tubular system. The tubular system consists of three parts: The first part of the tubular system, called the proximal tubule passes through the second part, Henle’s loop into the third part, the distal tubule. Proximal and distal tubule run parallel.
In the proximal tubule, important filtered-out components are first recovered. Here, about 2/3 of the filtered-out water is reabsorbed, i.e. returned to the body. A large proportion of salts and mineralsA mineral, in the context of nutrition, is an essential element (one that can only be obtained from the diet), required to perform functions necessary for life in the body.... (such as potassium, calcium), bicarbonate, sugar and phosphate are also transferred back into the blood here. On the other hand, substances such as medicines can also be actively excreted into the urine.
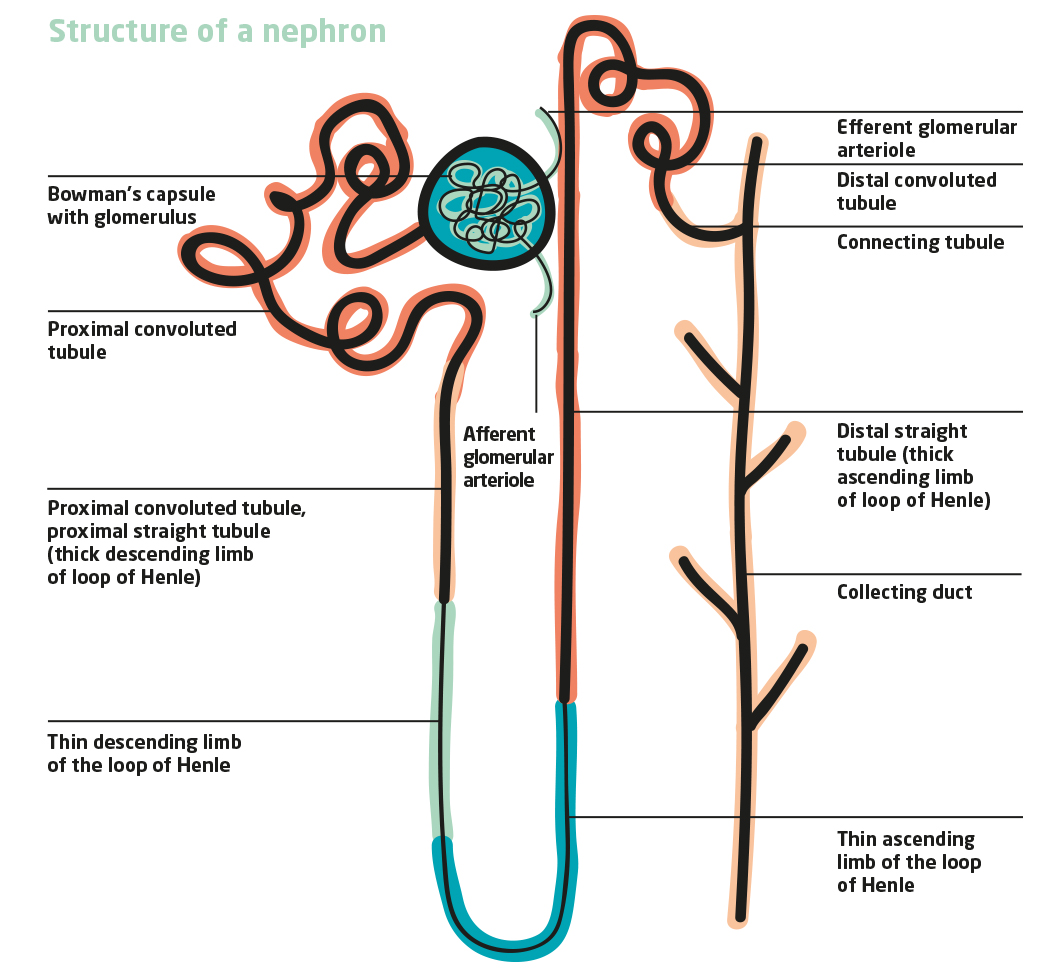
The proximal tubule passes into the loop of Henle, which runs through the renal medulla. Water is further recovered here, making the urine more concentrated (see specific gravity of urine). Saline and minerals such as calcium and magnesium can also be recovered in this area of the nephron. On the other hand, potassium can be actively excreted into the urine.
In the distal tubule, which adjoins Henle’s loop, the regulation of the water and electrolyte balance and the blood pH takes place under the influence of hormones. Here, too, water, common salt, magnesium, potassium and also urea are recovered.
Concentration of urine through water recovery
The urine becomes increasingly concentrated as more and more water is removed from it. Ultimately, only about 1% of the water filtered out of the glomerulum is excreted in the urine. 99% is reabsorbed in the nephron. This ability to concentrate urine by reabsorbing the water filtered out is lost in feline chronic kidney disease (CKD) due to damage and decay of the nephrons. This can be measured by the specific gravity of the urine, which decreases in CKD because more water is excreted and the urine can therefore no longer be concentrated.
Only about 1% of the water filtered out of the glomerulum is excreted in the urine. 99% is reabsorbed in the nephron.
The distal tubule finally merges into the collecting duct, which also runs parallel to the tubular system of the nephron. The collecting tube collects the urine and drains it into the renal pelvis. Blood vessels run parallel to all tubular structures and carry away the recovered water. Thus, the tubular systems and the blood vessels form a physical countercurrent principle. This makes it possible for an exchange of molecules to take place in the adjacent structures. The basic prerequisite for this is the parallel course of the structures with opposite flow directions of urine or blood.
Nephrons as hormone producers
The nephrons produce hormones that are involved in blood formation, bone metabolism and blood pressure regulation.
The hormone erythropoietinErythropoietin, abbreviated to EPO, is a growth factor that stimulates red blood cell production. EPO can be produced biotechnologically and administered for kidney failure or after chemotherapy...., contributes to blood formation by increasing the number of red blood cells (erythrocytesErythrocytes are red blood cells and contain the blood pigment haemoglobin. Red blood cells are responsible for transporting oxygen from the lungs into the cells of the tissues. They are predominantly produced in the bone marrow of larger bones....). Red blood cells transport vital oxygen. If the amount of oxygen in the kidney vessels decreases, more erythropoietin is released from the nephrons. In CKD, this hormone production decreases, so that affected cats tend to anemiaA blood deficiency. Anaemia is, effectively, reduced levels of the red blood pigment haemoglobin. Since this occurs in red blood cells (erythrocytes), a lack of red blood cells (erythrocytes) is often associated with a lack of blood pigment. The blood pigment transports oxygen in the.... With the consequence of pallor, weakness and fatigue.
As another important hormone, the nephrons produce calcitriolCalcitriol is the active form of vitamin D3. It is synthesised in the kidney from vitamin D. It is independently activated by three factors: increased parathyroid hormone levels, reduced calcium levels or indirectly via reduced phosphate levels. Calcitriol acts on four organs: 1) Bones: It..., the active form of vitamin D.
Calcitriol finely regulates the calcium-phosphate balance. If changes occur, calcium can be mobilized from the bone. If this pathway is activated excessively, as in renal disease, then this leads to the bone becoming demineralised and thus easily brittle. This problem occurs in conjunction with excessive phosphate blood levels (hyperphosphatemia). A too high phosphate level is the result of a reduced filtration capacity of the nephrons. An increased phosphate value can then be detected in the blood.
High blood pressure promotes glomerular filtration
If the blood pressure in the supplying vessel of the glomerulus is too low, the hormone reninA hormone-like enzyme, generated and stored in the kidneys. If blood pressure drops, it is released from the kidneys and is highly efficient in raising blood pressure.... is released by the kidneys, which contributes to an increase in blood pressure via a cascade (renin-angiotensin-aldosterone system). This fine regulation of blood pressure is disturbed in CKD. Since only a few nephrons can still function, in this case an increased blood pressure in the glomerula is regulated by the kidneys. This allows the remaining nephrons to filter out more. Their performance (glomerular filtration) initially increases. However, due to the overload, these nephrons also eventually perish. The increased blood pressure also causes proteins to be excreted into the urine that cannot be recovered in the downstream tubular systems due to the damage. As a result, more proteins are excreted in the urine, which becomes visible as proteinuria on the basis of the UPC.
CKD = nephrons decline
In feline chronic kidney disease (CKD), the nephrons lose their ability to excrete and detoxify, recover water and minerals, and produce hormones. The nephrons of the kidneys are limited in number. Cats, for example, have 200,000 nephrons. Humans have about ten times more. Damaged nephrons do not recover. They perish.
The CKD leads via different vicious circles to the fact that more and more nephrons die and thus their tasks are carried out more and more badly. Nevertheless, the first symptoms of CKD only appear when 2/3 to ¾ of the nephrons have already been irretrievably destroyed. The remaining nephrons are true power plants, which can maintain their detoxification and excretion work as well as their regulation of water, blood pH and minerals and their hormone production amazingly well via finely tuned mechanisms: Frequently, no evidence of kidney damage is visible even in the blood count, which is, after all, a mirror for the filtration work of the nephrons. Nevertheless, preservation of the existing nephrons is the top priority in CKD in order to slow down the progressive process of chronic kidney disease. To this end, it is necessary to break the existing vicious circles.
Read more about four vicous cycles of chronic kidney disease.
Bibliography
- Brandes, R., Lang, F. & Schmidt, R. F. (2020): Physiologie des Menschen – mit Pathophysiologie, 32. Auflage, Springer-Verlag, Berlin.
- Nieder, C. (2021): CNE Chronische Nierenerkrankung der Katze – erklärt für Katzenfreunde, BoD, Books on Demand, Norderstedt


