
IRIS Stages
Staging= Classification of the cat into a stage of chronic kidney disease according to IRIS... is the classification of the cat into one of four IRIS stages and determines the severity of the chronic kidney disease. A stage is also linked to a prognosis. IRIS recommends specific treatments and procedures depending on the stage. However, the diagnosis of “chronic kidney disease” must first be confirmed using the IRIS recommendations.
Once diagnosed, the four main stages are classified based on blood creatinineCreatinine is a breakdown product of muscle metabolism. Its blood level is dependent, among many factors, on age, weight, nutritional status and muscle mass. Hence, creatinine levels in the blood vary from individual to individual. Creatinine is continuously excreted in the urine. Increased blood creatinine... (the cat must have been fasted beforehand). Simultaneous measurement of SDMASDMA = Symmetrical Dimethylarginine, which is a degradation product of the amino acid arginine and is excreted solely through the kidneys. SDMA is a highly specific biomarker for kidney function in cats. Read more: SDMA test (blood test)... is also recommended. A stable creatinine and SDMA level (> 14 µg/dl) is a prerequisite for staging. Plasma or serum creatinine is considered stable if the variation between at least two measurements taken 2-4 weeks apart is less than 20-25 %. There should also be a stable UP/C and specific urine weight.
In addition, there are four further sub-stages depending on the blood pressure and a further 3 sub-stages based on the presence of proteinuriaIncreased protein in urine, leading to loss of protein. Normally, only a very small amount of protein is excreted in the urine. In chronic kidney disease, the amount lost may increase. High blood pressure damages blood vessels in the nephrons making them more permeable and....
This categorisation facilitates the diagnosis, communication and treatment of chronic kidney disease in cats.
IRIS staging is based on the creatinine blood level. SDMA is used to assist in staging.
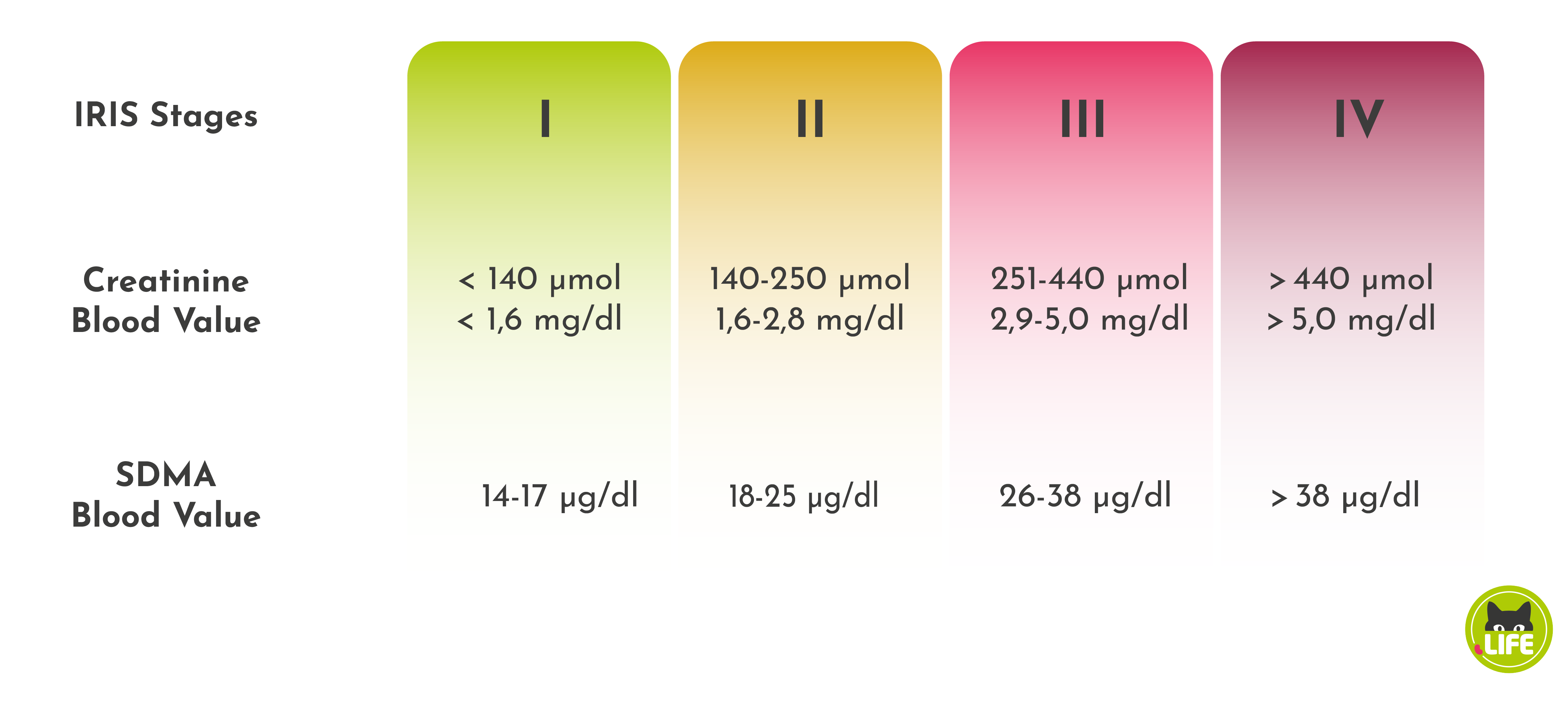
If there is a discrepancy between the staging based on SDMA and creatinine, the muscularity of the cat should be considered. Both measurements should be repeated after approximately 14 days. If there is still a discrepancy between the two values, the higher stage indicated by one of the values, usually the SDMA value, should be used.
Skip directly to
Stage I
In stage 1, blood creatinine is usually within normal range (<140 μmol/L or <1.6 mg/dl). SDMA is <18 μg/dl but always >14 μg/dl in several samples. It becomes noticeable that the cat has lost 5-10 % of its body weight and the specific gravity of the urine is below the threshold of 1.035, which means that the density of the urine decreases and the kidneys cannot concentrate the urine as effectively.
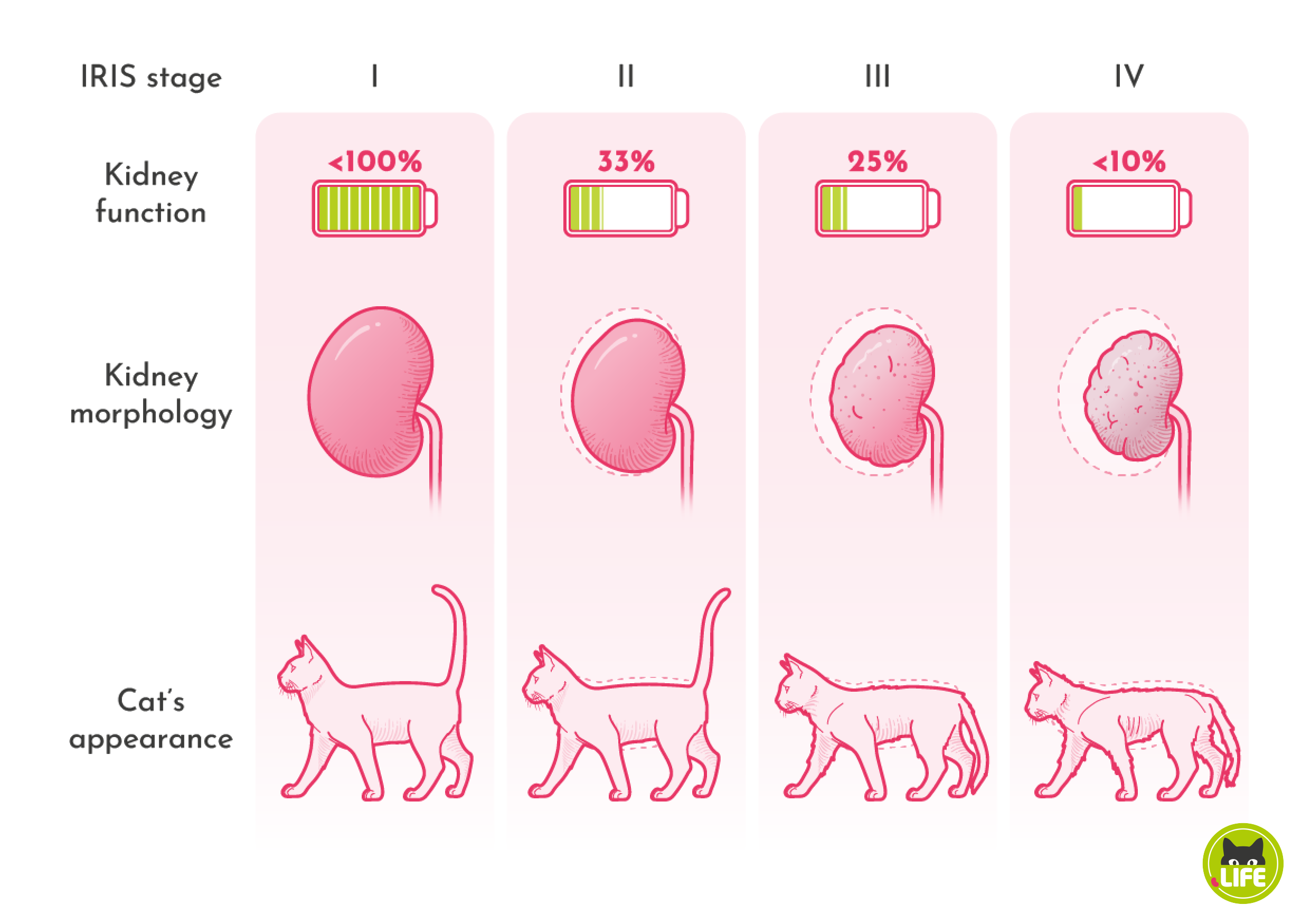
Stage I is often difficult to diagnose because the blood creatinine level is still within the reference range. The presence of CKD is indicated by a 15-20 % increase in the cat’s individual creatinine level within the normal range. In order to assess this individual blood creatinine level, it is recommended that cats over 7 years of age are examined (urine and blood test) at least once a year. Cats in stage I have very few clinical signs and although overall kidney function is reduced due to a decrease in the number of functioning nephronsNephrone sind die Filtereinheiten der Nieren...., it is still well over 60 % and the deficiencies can be largely compensated for.
In cats with CKD, high blood pressure can occur as early as stage I. Protein is usually found in the urine as the increased blood pressure causes proteins to be extruded This is called proteinuria and is measured by UP/C in the urine. Both blood pressure and proteinuria are categorised into sub-stages by IRIS.
In stage I, clinical changes are barely noticeable. There may be a slight increase in thirst with a slight increase in drinking (polydipsiaExcessive thirst due to illness, leading to excessive production of urine (polyuria)....) and a corresponding increase in urination (polyuriaExcessive production of urine, potentially due to kidney failure....). Signs of fatigue, increased need for sleep and tiredness are attributed to the age of the cat and are therefore rarely recognised. The slight weight loss of 5-10 % will only become apparent if the cat’s weight has been recorded over a long period (preferably several years) using a suitably accurate scale (not the usual household scales for humans, but baby scales).
Factors triggering CKD should be identified and, if possible, eliminated at this stage. Caution should be exercised when using medications that can damage the kidneys. You should carefully monitor and encourage your cat to drink.
Stage II
In stage II, the kidneys are only able to work at about 1/3 of their capacity. Many urinary substances accumulate in the blood. The reduced excretion leads to changes in the blood count. In the second stage, blood creatinine levels are slightly elevated. At this stage, the creatinine level is 140-250 μmol/l or 1.6-2.8 mg/dl and may still be at the upper limit of reference range. An increase of 15-20 % in the individual creatinine value is in itself a sign of impaired kidney function, not that the upper limit of the normal range specified by the laboratory has been exceeded. The SDMA level, which rises earlier than the blood creatinine level, can also be of help. In the second stage of CKD, the blood concentration of SDMA is 18-25 μg/dl, which is also slightly elevated. The urine test will usually show a UP/C (urine protein to creatinine ratio) above 0.4, which according to IRIS corresponds to proteinuria (= loss of protein in the urine). Blood pressure should be checked and, if elevated, treated with appropriate medication. Blood phosphate levels must be monitored and kept below 1.5 mmol/l by using phosphate binders and/or phosphate-reduced foods (kidney-friendly diets). Treatment focuses on slowing the progression of CKD. At this stage, cats still have a chance of survival of more than three years.
Metabolic waste products and uraemic toxinsToxic, nitrogen-containing urinary substances responsible for uraemia and kidney damage.... are retained and the first clinical symptoms become more evident In stage II, increased drinking (polydipsia) becomes more apparent. Vomiting or diarrhoea may also occur. Loss of appetite, drowsiness and weight loss are more pronounced.
Stage III
In stage III, blood levels are well above the normal range and clinical symptoms increase. Renal function is still around ¼, while 75 % of renal function has been irretrievably lost. The process of further nephron destruction via increased blood pressure, accumulated phosphate and accumulated uraemic toxins is well underway. The progression of CKD is clearly visible.
Not only the blood count shows significant changes, such as an increase in the blood creatinine level to a value of 251-440 μmol/l or 2.9-5.0 mg/dl and the blood SDMA value of 26-38 μg/dl. The clinical symptoms and progression of the disease are significantly influenced by the reduced excretion of toxic waste products of protein metabolism, such as uremic toxins and in particular indoxyl sulphate.
Phosphate is also retained and accumulates in the blood. This leads to hyperphosphatemia. This sets in motion a vicious cycle of further kidney destruction, which, through the activation of parathyroid hormoneParathyroid hormone (PTH) is a hormone secreted by the parathyroid glands, which regulates calcium levels in the blood. PTH is secreted in response to low blood calcium levels (hypocalcaemia). An increase in calcium concentration above the normal value inhibits PTH production (negative feedback). PTH stimulates..., leads to a variety of problems in CKD and can also lead to clinical symptoms. As the kidneys are unable to excrete enough phosphate, phosphate intake should be reduced. In most cases, a combination of phosphate binders and phosphate-reduced diets (kidney-friendly diets) is recommended to keep phosphate levels below 1.6 mmol/l at this stage.
If the blood becomes acidotic (metabolic acidosisIncreased acidity of the blood and the body. Metabolic acidosis occurs in chronic renal failure due to uraemia (raised blood urea) but can also have many other metabolic causes.... – low blood pH), this should be treated, as should high blood pressure and proteinuria. At this stage, fluids may be needed to maintain hydration. If the haematocrit falls below 20 %, treatment for anaemia is also advisable. The cat’s appetite, which is often severely reduced due to vomiting, nausea and gastric acidity, should be stimulated with medication if necessary to maintain the cat’s energy level. Renal support measures aim to slow the progression of CKD and improve quality of life by reducing clinical signs. Cats in stage III have a remaining life expectancy of about two years.
The clinical signs of uraemiaA raised level in the blood of urea and other urinary substances, which in chronic kidney disease can no longer be adequately excreted due to impaired renal function (glomerular filtration rate). This leads to renal damage due to uraemic toxins, toxic urinary substances The symptoms... are quite obvious. Weight loss is striking. Cats usually eat poorly, vomit and are reluctant to eat, even losing their appetite. The cat will sometimes try to satiate its increased thirst in unusual places, looking for water in flowerpots and sometimes in toilets. Frequent urination (= polyuria) can cause the cat to become unclean because it may not be able to reach the litter tray. Cats may become more fussy about their food, be reluctant to eat and have a reduced appetite. Changes in the mucous membranes of the mouth and gastrointestinal problems may occur. The cat will appear much less active. Cats usually also show anaemia and the mucosa becomes pale to milky-white. Up to 2 years is the average survival time.
Stage IV
Finally, in stage IV, the kidneys function at a minimum of less than 10 %. The process ends in fatal renal failureLoss of kidney function, which may be sudden (acute) or gradual (chronic), as in chronic kidney disease. Loss of kidney function leads to a reduced filtration capacity (glomerular filtration rate) and, thus, an inability to sufficiently filter out urinary substances such as uraemic toxins. Renal.... Cats in this stage show very clear symptoms. The blood values in the renal profile are all significantly elevated. Creatinine is over 440 μmol/l or over 5.0 mg/dl. The SDMA level rises to over 38 ug/dl. As a result of poor kidney function, waste products and toxins cannot be adequately excreted and accumulate in the blood. This leads to internal urinary intoxication, known as uremia, which is responsible for the clinical symptoms.
This last stage is characterised by progressive clinical symptoms that should be treated accordingly. Treatment should focus on alleviating clinical symptoms such as severe nausea, vomiting, loss of appetite, drowsiness, emaciation and dehydrationA deficit of total body water. Dehydration can be caused by excessive fluid loss, for instance via the kidneys in CKD, or by insufficient fluid intake..... In the fourth stage, advanced emaciation becomes very evident.
A deficit in total body fluids (= dehydration) can be caused by excessive fluid loss, e.g. through the kidneys in CKD, or by inadequate fluid intake. Cats usually become dehydrated because the kidneys are no longer able to concentrate urine and recover water, so the cat excretes too much water through the kidneys.
HypertensionHigh blood pressure. (due to its harmful effects on vision, such as retinal detachment and even blindness) and anaemia must be treated with medication, and metabolic acidosis must be controlled. Due to the increased phosphate content and the retained uraemic toxins, clinical symptoms such as plantigrade gaitA “bear-like” gait. Cats walking with a plantigrade gait don’t walk on their paw tips, but with their metatarsal bones and hocks (ankles) on the ground. Typically occurs in cats with diabetes.... become increasingly apparent. The cat walks on its hocks and shows weakness of the hindquarters. The cat’s interaction with its owner is limited, the cat appears apathetic and may even go blind due to high blood pressure. The cat’s quality of life will be significantly reduced, indicating that the cat is not doing well. Phosphate levels should be kept below 1.9 mmol/l with phosphate-reduced foods and phosphate binders. The aim is to make the remaining (on average) one to three months of the cat’s life as enjoyable as possible.
Many dogs and cats with CKD progress through all four stages, but some, particularly geriatric cats, have non-progressive or minimally progressive kidney disease. These patients may remain in an IRIS stage and another disease may become the more clinically significant and life-limiting problem.
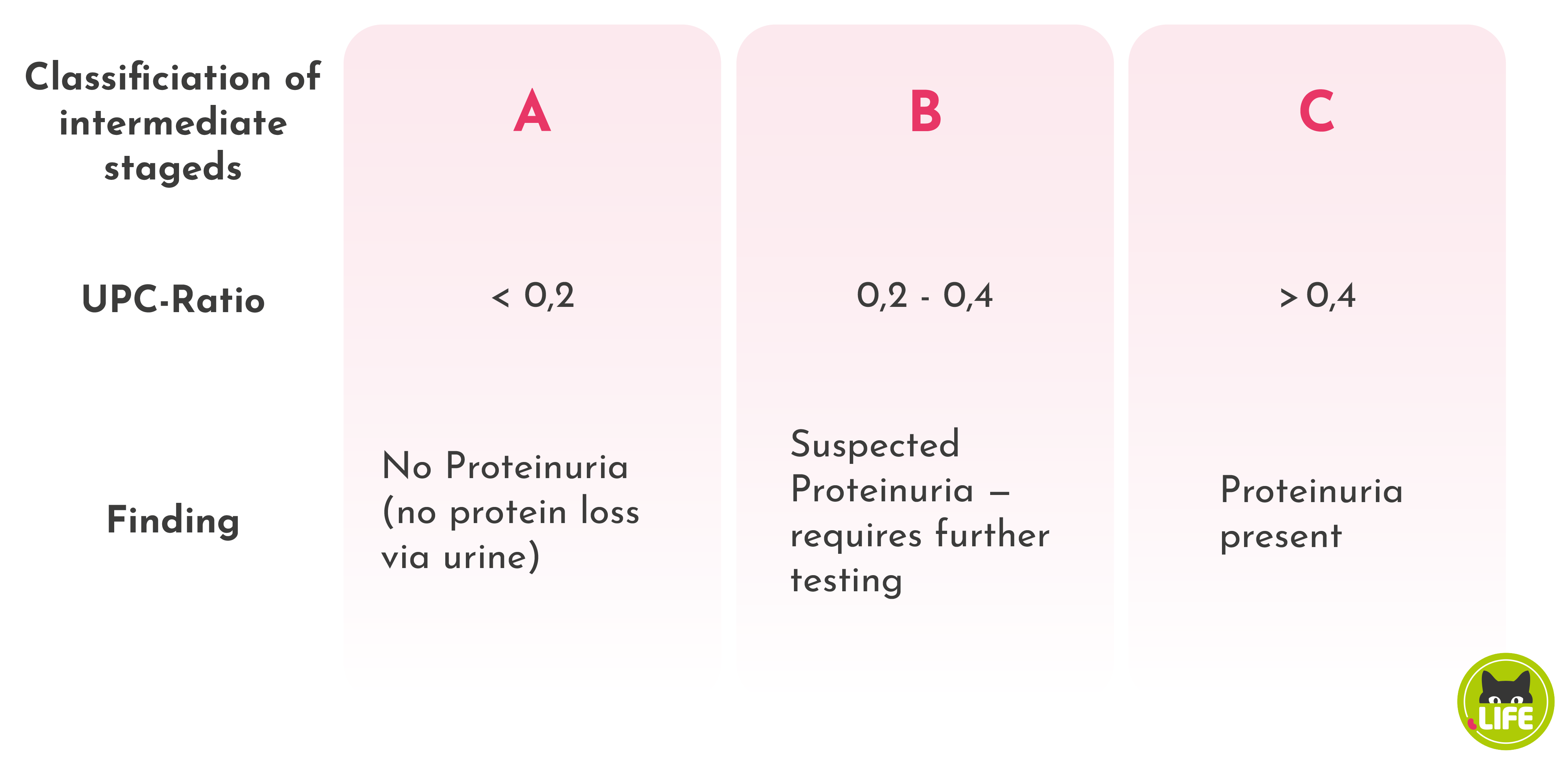
Sub-stages of proteinuria
Measurements of proteinuria using the urine protein to creatinine ratio, also known as UP/C, should also be repeated at 10-14 day intervals to confirm a stable condition. Single measurements can be misleading because proteinuria can have several causes, including inflammatory changes in the kidneys, bladder or ureters. Therefore, if proteinuria is present, further laboratory tests of urine and blood must be carried out to clarify the causes of proteinuria.
Approximately 20 % of cats with CKD will develop proteinuria. Proteinuria, like hypertension, is involved in the progression of kidney damage and therefore needs to be treated.
Hypertension and proteinuria are linked.
Loss of protein (proteinuria) is usually associated with high blood pressure. Normally, proteins remain in the blood and are not filtered out. However, with increased filtration pressure, i.e. high blood pressure, more and more proteins pass into the urine. When this happens in a healthy kidney, most proteins are recovered in the nephron. In a damaged kidney, however, this does not happen sufficiently.
Sub-stages based on blood pressure
Blood pressure plays an important role in the progression of the disease, but also in the clinical symptoms. As the kidneys are involved in the regulation of blood pressure, they are also affected by the progressive loss of nephrons. The result is high blood pressure. Initially, this is a compensation for the reduced kidney function. If less can be filtered because nephrons are missing, increased blood pressure leads to increased filtration pressure, which initially compensates for reduced kidney function. However, the increased blood pressure overloads the remaining nephrons, which are then destroyed. The result is a vicious cycle of compensation, overburdening and further nephron destruction.
Increased blood pressure also affects other organs, resulting in clinical symptoms. For example, hypertension can lead to retinal detachment, which can cause blindness in cats. Cats with high blood pressure often show dilated pupils, nictitating membrane prolapse or press their heads against objects. In the brain, high blood pressure can increase the risk of stroke.
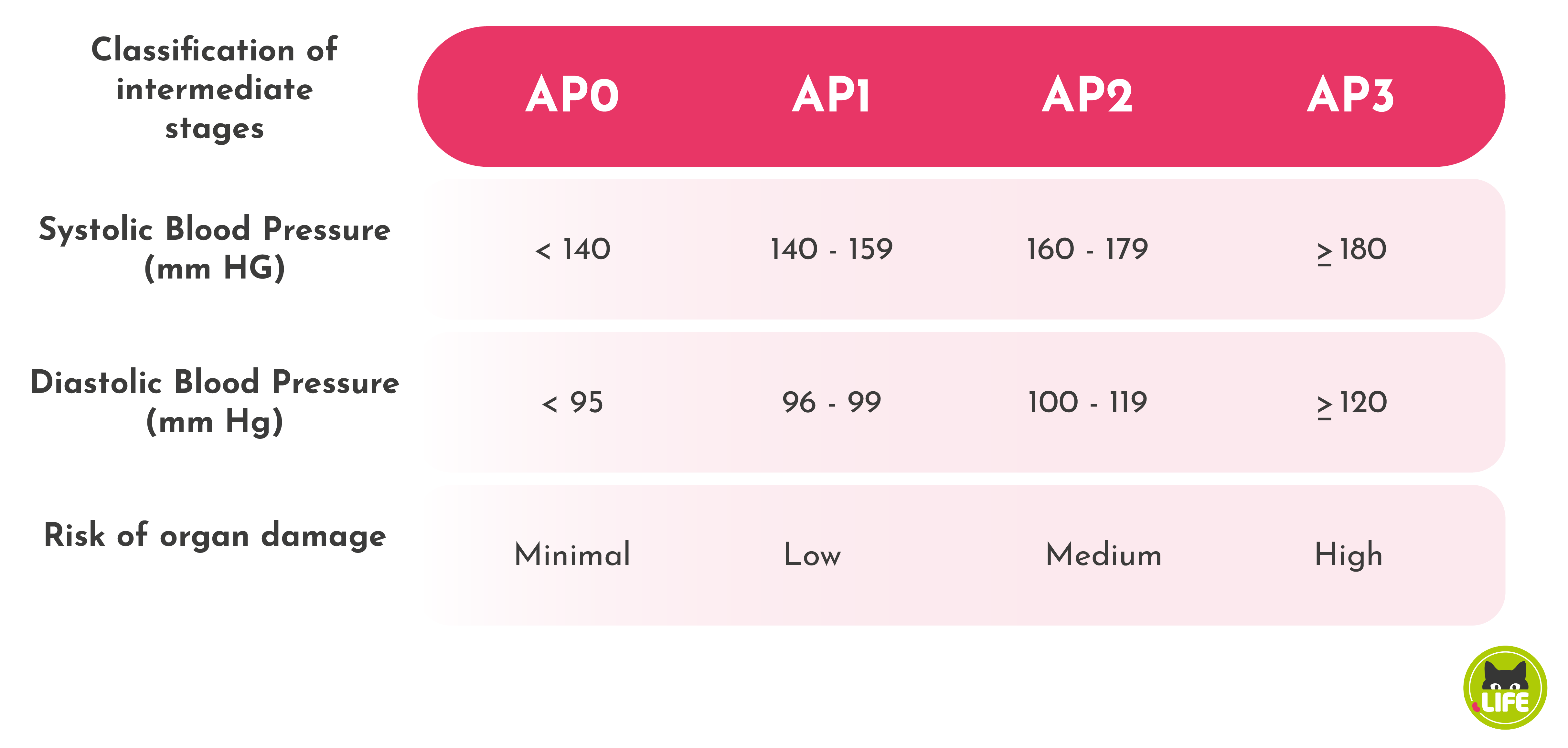
For moderate hypertension, antihypertensive therapy is recommended if there is a risk of organ damage, for example to the eye. For severe hypertension, antihypertensive medication is always indicated. The goal of treatment is a systolic blood pressure in the range of 150 – 160 mm Hg. In stage IV, the target blood pressure may be somewhat higher because the blood pressure represents the filtration pressure and the minimally functioning kidney will go into fatal kidney failure more quickly if the blood pressure drops. It is therefore possible that blood levels of creatinine, ureaUrea is the nitrogen-containing breakdown product of protein metabolism. The nitrogen from the proteins is converted to ammonia in the liver, which is combined with carbon dioxide to form urea. This is continuously excreted via the kidneys but also via sweat. Urea is one of... and SDMA may rise during antihypertensive treatment.
