
Three fundamental treatment goals:
Treat the causes of CKD
Reduce the causes of chronic kidney disease (CKD) as far as possible.
Slow the progression (extending life)
Stabilise kidney function and slow down progression by breaking the vicious circles.
Improve quality of life
Provide treatment and improve the symptoms of CKD accompanying diseases.
TREATMENT OF CKD
Understanding how to treat CKD relies on knowledge of the interactions between the individual disease-causing (pathogenic) factors. In this chapter I focus on the principles underlying CKD treatment, before presenting the therapeutic guidelines of the International Renal Interest Society (IRIS) for each stage of the disease.
There is no single treatment for CKD; treatment is based on breaking the individual vicious circles that contribute to the disease’s progression and on managing individual symptoms. It’s important, however, to understand the basic principles.
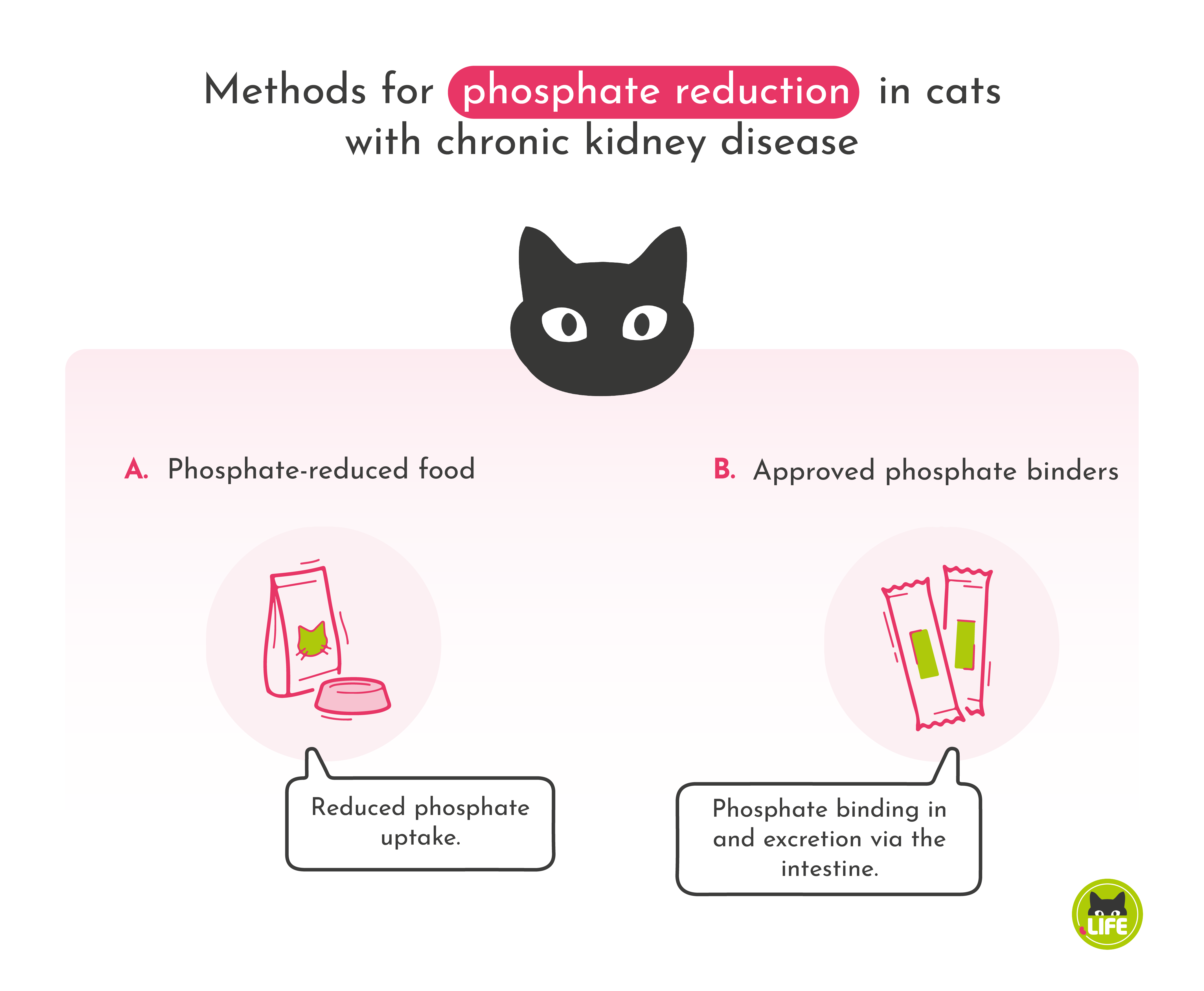
LOWERING PHOSPHATE
 In particular, this involves reducing the phosphate in cat food. This can be achieved in two ways. First, by reducing phosphate in the food itself. This is done by replacing meat protein with plant protein, usually wheat gluten, as meat contains a lot of phosphate (kidney-friendly food). Cats aren’t plant eaters, so usually they don’t particularly enjoy eating this kind of food. Another alternative is to bind the existing phosphate in the gut so it is eliminated with the faeces. This is achieved by “phosphate binders” (usually based on calcium carbonate), which are added to the cat food.
In particular, this involves reducing the phosphate in cat food. This can be achieved in two ways. First, by reducing phosphate in the food itself. This is done by replacing meat protein with plant protein, usually wheat gluten, as meat contains a lot of phosphate (kidney-friendly food). Cats aren’t plant eaters, so usually they don’t particularly enjoy eating this kind of food. Another alternative is to bind the existing phosphate in the gut so it is eliminated with the faeces. This is achieved by “phosphate binders” (usually based on calcium carbonate), which are added to the cat food.
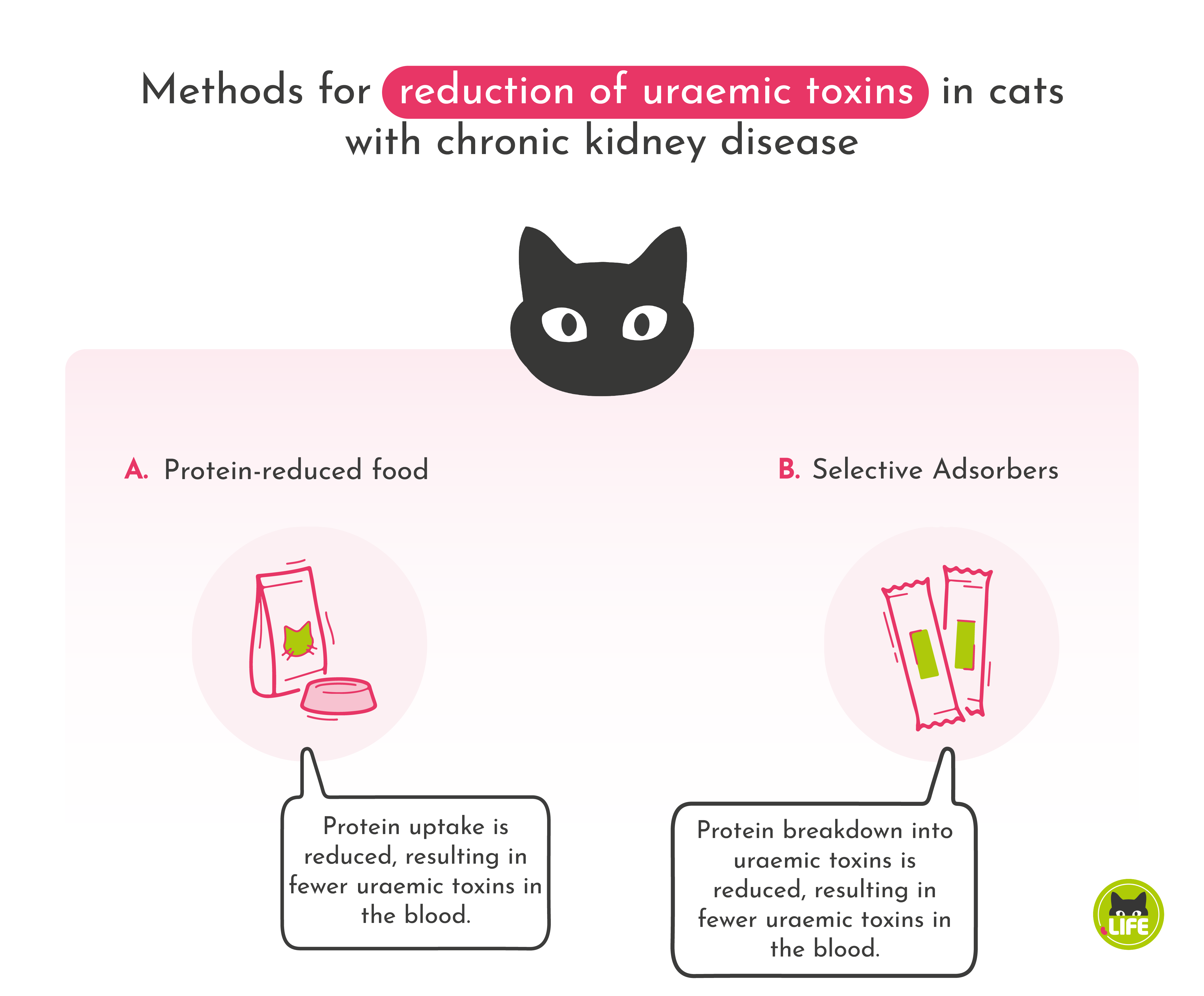
REDUCTION OF PROTEIN
The protein content of food is reduced to lower levels of uraemic toxins. In the intestines, bacteria generate the precursors of uraemic toxin from proteins. These are then absorbed and converted into actual uraemic toxinsToxic, nitrogen-containing urinary substances responsible for uraemia and kidney damage.... in the liver. These need to be excreted by the kidneys. However, reduction of protein in food as a therapeutic option is disputed, as cats depend on protein as an energy source (see: cats as obligatory carnivores). A better approach is to eliminate factors that trigger uraemiaA raised level in the blood of urea and other urinary substances, which in chronic kidney disease can no longer be adequately excreted due to impaired renal function (glomerular filtration rate). This leads to renal damage due to uraemic toxins, toxic urinary substances The symptoms... (accumulation of uraemic toxins in the blood) and thus symptoms at an early stage by binding their precursors already in the intestines. In principle, it is naturally also better for the kidneys if less urinary substances are excreted, and this can be supported, for example, by the use of oral dialysis to lower levels of uraemic toxins.
REDUCTION OF BLOOD PRESSURE
The kidneys are organs that can regulate their own blood pressure (“autoregulation” of kidney blood flow). They have a variety of mechanisms at their disposal to help them do so. The filtration rate of individual nephronsNephrone sind die Filtereinheiten der Nieren.... is dependent on blood pressure. The rate increases with higher blood pressure. However, persistent high blood pressure can also harm the kidneys. It results in overburdening and hardening of the blood vessels (“sclerosisThe hardening of an organ or tissue caused by a replacement of normal tissue with connective tissue. Sclerotic tissues and organs are less elastic....”: a hardening of the vessels due to proliferation of connective tissue), due to the lack of protective substances. This leads to progressive damage of the vascular system of the nephrons and eventually to their destruction. Twenty per cent of CKD cats develop high blood pressure at an early stage. However, there are indications that this figure is actually much higher.
High blood pressure can lead to a variety of clinical symptoms: central nervous disorders such as seizures, cramps, lethargy, strokes, difficulty in walking, visual disturbances, and even blindness due to a retinal detachment.
High blood pressure also leads to an increase in proteins in the filtrate, and these can no longer be reabsorbed, leading to increased protein in the urine (proteinuriaIncreased protein in urine, leading to loss of protein. Normally, only a very small amount of protein is excreted in the urine. In chronic kidney disease, the amount lost may increase. High blood pressure damages blood vessels in the nephrons making them more permeable and...). CKD progression can be slowed down by reducing blood pressure and, with it, proteinuria.
Reduction of proteinuria
As proteinuria is usually caused by high blood pressure, proteinuria and high blood pressure can be reduced together (it is important, however, to establish that the cause of the proteinuria are really the kidneys). To do so, cats are given targeted medication, usually in food as tablets or as liquid suspensions.
Reduction of individual symptoms
The symptoms of CKD vary from cat to cat and need to be treated individually. Reducing uraemia and blood pressure, alone, can improve many symptoms.
It’s critically important, in spite of nausea, vomiting and loss of appetite, that your cat eats well. You should try and improve the attractiveness of food, for instance by warming it up and serving small portions several times a day. If your cat’s appetite doesn’t improve, medicines that stimulate appetite and/or reduce stomach acid can also help.
To encourage your cat to drink, provide it with a choice of fresh water sources, possibly including a fresh water fountain, or add a few drops of tuna oil to the water to make it more appealing.

